Thursday, November 27, 2014
Sunday, November 2, 2014
FUNDACIÓN ESPERANZA SEMAJORIE
La sarcoidosis es una enfermedad autoinmune que puede
afectar a cualquier órgano en su cuerpo, así como su piel. No hay ninguna cura
conocida. No se ha probado si esta enfermedad se deriva de los genes
hereditarios o el medio ambiente. Nuestra meta es tener salud servicios
gratuitos en todo el país que detectarán esta enfermedad autoinmune, así como
otros. Ayudar a nuestras comunidades para elegir una suficiente cobertura de
seguro de salud para sus familias. Proveer transportación médica a estas
instalaciones, así como el cuidado de guardería y de hospicio asequible. Únete
a la lucha contra la Sarcoidosis. LA CINTA MORADA Y A APOYAR LA CAUSA - https://www.paypal.com/cgi-bin/webscr?cmd=_s-xclick&hosted_button_id=FBDM8MTWS8JJY
Monday, October 20, 2014
Saturday, September 27, 2014
Tuesday, August 26, 2014
Thursday, August 21, 2014
Wednesday, August 20, 2014
Where can I find additional information about beta thalassemia?
You may find the following resources about beta thalassemia helpful. These materials are written for the general public.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
- MedlinePlus - Health information (3 links)
- Genetic and Rare Diseases Information
Center - Information about genetic conditions and rare diseases - Additional NIH Resources - National Institutes of Health (2 links)
- Educational resources - Information pages (15 links)
- Patient support - For patients and families (6 links)
- Gene
Reviews - Clinical summary - Genetic Testing Registry - Repository of genetic test information (2 links)
ClinicalTrials.gov - Linking patients to medical researchPubMed - Recent literature- OMIM - Genetic disorder catalog (3 links)
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
Tuesday, August 19, 2014
Monday, July 14, 2014
Where Can I Find Information About Diagnosis Or Management Of Beta Thalassemia?
These resources address the diagnosis or management of beta thalassemia and may include treatment providers.
General information about the diagnosis and management of genetic conditions is available in the Handbook. Read more about genetic testing, particularly the difference between clinical tests and research tests.
To locate a healthcare provider, see How can I find a genetics professional in my area? in the Handbook.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
- Gene Review:
Beta-Thalassemia - Genetic Testing Registry: beta
Thalassemia - Genetic Testing Registry: Beta-thalassemia, dominant inclusion body
type - MedlinePlus Encyclopedia:
Thalassemia
General information about the diagnosis and management of genetic conditions is available in the Handbook. Read more about genetic testing, particularly the difference between clinical tests and research tests.
To locate a healthcare provider, see How can I find a genetics professional in my area? in the Handbook.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
How Do People Inherit Beta Thalassemia?
Thalassemia major and thalassemia intermedia are inherited in an autosomal recessive pattern, which means both copies of the HBB gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. Sometimes, however, people with only one HBB gene mutation in each cell develop mild anemia. These mildly affected people are said to have thalassemia minor.
In a small percentage of families, the HBB gene mutation is inherited in an autosomal dominant manner. In these cases, one copy of the altered gene in each cell is sufficient to cause the signs and symptoms of beta thalassemia.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
In a small percentage of families, the HBB gene mutation is inherited in an autosomal dominant manner. In these cases, one copy of the altered gene in each cell is sufficient to cause the signs and symptoms of beta thalassemia.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
What Genes Are Related To Beta Thalassemia?
Mutations in the HBB gene cause beta thalassemia. The HBB gene provides instructions for making a protein called beta-globin. Beta-globin is a component (subunit) of hemoglobin. Hemoglobin consists of four protein subunits, typically two subunits of beta-globin and two subunits of another protein called alpha-globin.
Some mutations in the HBB gene prevent the production of any beta-globin. The absence of beta-globin is referred to as beta-zero (B0) thalassemia. Other HBB gene mutations allow some beta-globin to be produced but in reduced amounts. A reduced amount of beta-globin is called beta-plus (B+) thalassemia. Having either B0 or B+ thalassemia does not necessarily predict disease severity, however; people with both types have been diagnosed with thalassemia major and thalassemia intermedia.
A lack of beta-globin leads to a reduced amount of functional hemoglobin. Without sufficient hemoglobin, red blood cells do not develop normally, causing a shortage of mature red blood cells. The low number of mature red blood cells leads to anemia and other associated health problems in people with beta thalassemia.
Read more about the HBB gene.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
Some mutations in the HBB gene prevent the production of any beta-globin. The absence of beta-globin is referred to as beta-zero (B0) thalassemia. Other HBB gene mutations allow some beta-globin to be produced but in reduced amounts. A reduced amount of beta-globin is called beta-plus (B+) thalassemia. Having either B0 or B+ thalassemia does not necessarily predict disease severity, however; people with both types have been diagnosed with thalassemia major and thalassemia intermedia.
A lack of beta-globin leads to a reduced amount of functional hemoglobin. Without sufficient hemoglobin, red blood cells do not develop normally, causing a shortage of mature red blood cells. The low number of mature red blood cells leads to anemia and other associated health problems in people with beta thalassemia.
Read more about the HBB gene.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
How Common Is Beta Thalassemia?
Beta thalassemia is a fairly common blood disorder worldwide. Thousands of infants with beta thalassemia are born each year. Beta thalassemia occurs most frequently in people from Mediterranean countries, North Africa, the Middle East, India, Central Asia, and Southeast Asia.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
What is Beta Thalassemia?
Beta thalassemia is a blood disorder that reduces the production of hemoglobin. Hemoglobin is the iron-containing protein in red blood cells that carries oxygen to cells throughout the body.
In people with beta thalassemia, low levels of hemoglobin lead to a lack of oxygen in many parts of the body. Affected individuals also have a shortage of red blood cells (anemia), which can cause pale skin, weakness, fatigue, and more serious complications. People with beta thalassemia are at an increased risk of developing abnormal blood clots.
Beta thalassemia is classified into two types depending on the severity of symptoms: thalassemia major (also known as Cooley's anemia) and thalassemia intermedia. Of the two types, thalassemia major is more severe.
The signs and symptoms of thalassemia major appear within the first 2 years of life. Children develop life-threatening anemia. They do not gain weight and grow at the expected rate (failure to thrive) and may develop yellowing of the skin and whites of the eyes (jaundice). Affected individuals may have an enlarged spleen, liver, and heart, and their bones may be misshapen. Some adolescents with thalassemia major experience delayed puberty. Many people with thalassemia major have such severe symptoms that they need frequent blood transfusions to replenish their red blood cell supply. Over time, an influx of iron-containing hemoglobin from chronic blood transfusions can lead to a buildup of iron in the body, resulting in liver, heart, and hormone problems.
Thalassemia intermedia is milder than thalassemia major. The signs and symptoms of thalassemia intermedia appear in early childhood or later in life. Affected individuals have mild to moderate anemia and may also have slow growth and bone abnormalities.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
In people with beta thalassemia, low levels of hemoglobin lead to a lack of oxygen in many parts of the body. Affected individuals also have a shortage of red blood cells (anemia), which can cause pale skin, weakness, fatigue, and more serious complications. People with beta thalassemia are at an increased risk of developing abnormal blood clots.
Beta thalassemia is classified into two types depending on the severity of symptoms: thalassemia major (also known as Cooley's anemia) and thalassemia intermedia. Of the two types, thalassemia major is more severe.
The signs and symptoms of thalassemia major appear within the first 2 years of life. Children develop life-threatening anemia. They do not gain weight and grow at the expected rate (failure to thrive) and may develop yellowing of the skin and whites of the eyes (jaundice). Affected individuals may have an enlarged spleen, liver, and heart, and their bones may be misshapen. Some adolescents with thalassemia major experience delayed puberty. Many people with thalassemia major have such severe symptoms that they need frequent blood transfusions to replenish their red blood cell supply. Over time, an influx of iron-containing hemoglobin from chronic blood transfusions can lead to a buildup of iron in the body, resulting in liver, heart, and hormone problems.
Thalassemia intermedia is milder than thalassemia major. The signs and symptoms of thalassemia intermedia appear in early childhood or later in life. Affected individuals have mild to moderate anemia and may also have slow growth and bone abnormalities.
Referenced from http://ghr.nlm.nih.gov/condition/beta-thalassemia
Wednesday, July 2, 2014
Friday, June 27, 2014
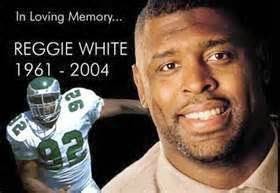
Famous People With Sarcoidosis
Mahalia Jackson - Gospel Singer
Bill Russell - American Basketball Player
Floyd Mayweather Sr. - Ex Boxer/Trainer
James E. Ray - Basketball Player
Manning Marable - Author
Bernie Mac - Comedian
Angie Stone - Singer
Mathew Good - Singer
Reggie White - American Football Player
Daisy Fuentes - Actress/Model
Karen Duff - Actress/Model
Darrian Chapman - Sportscaster NBC5
Sean Le Vert - R&B Singer
Tisha Campbell-Martin - Actress/Model
Daryl Hawks - Sportscaster NBC5
Travis Michael Holder - Actor
Van Ludwig Beethoven - Musician
Evander Hollyfield - Boxer
Sunday, June 22, 2014
Understanding Cystic Fibrosis
Cystic fibrosis is a genetic disease, meaning it is caused by a person's genes. It affects the glands that produce mucus and sweat, causing mucus to become thick and sticky.
As the mucus builds up, it can block airways in the lungs. This makes it increasingly difficult to breathe.
Mucus buildup also makes it easier for bacteria to grow. This can cause frequent infections in the lungs.
Mucus buildup can prevent necessary digestive enzymes from reaching your intestines. The body needs these enzymes to digest the nutrients in the food that you eat, including fats and carbohydrates.
People with cystic fibrosis also lose large amounts of salt when they sweat. This can cause an unhealthy imbalance of minerals in your body. It can lead to:
- Dehydration
- Fatigue
- Weakness
- Increased heart rate
- Low blood pressure
- Heat stroke
- Death in rare cases
About 30,000 Americans have cystic fibrosis. Each year about 1,000 new cases are diagnosed.
Sixty years ago, the disease killed most people who had it before they reached elementary school. Nowadays people with cystic fibrosis have an average lifespan of about 37 years.
What Causes Cystic Fibrosis?
Cystic fibrosis is an inherited disease.
For someone to get cystic fibrosis, both parents must be carriers of the gene that causes it and then pass it on. That means 25% of the children of such parents will have cystic fibrosis.
Boys and girls are equally likely to get the disease. About 10 million Americans carry the gene and do not know it. More whites get the disease than do people of other races.
Monday, June 16, 2014
Early Detection of Cystic Fibrosis
Both newborns and adults can be tested for the changed (mutated) gene that causes cystic fibrosis. These tests include:
Article Referenced from WebMD
- Newborn screening. Levels of a type of digestive enzyme are measured from a blood sample. High levels of this enzyme suggest cystic fibrosis. Some newborns may also have a genetic test.
- Genetic test for adults. These tests identify the most common defects in the cystic fibrosis transmembrane regulator (CFTR) gene. Genetic testing can be done during pregnancy through chorionic villus sampling or amniocentesis. The test can also be done before pregnancy, to help couples find out if either or both of them carry a defective CFTR gene.
- If both parents carry the changed gene, there is a 25% (1-in-4) chance that their child will have no genetic problem. There is a 25% chance that their child will have cystic fibrosis. And there is a 50% (1-in-2) chance that their child will be a carrier.
- If only one parent is a carrier of the changed gene, the child will not have cystic fibrosis. But there is a 50% chance that the child will be a carrier.
Article Referenced from WebMD
Monitoring Cystic Fibrosis
Certain tests can help your doctor monitor your child's cystic fibrosis. These tests include:
- Lung function tests to find out how healthy the lungs are by checking how well air moves into and out of the lungs.
- A throat culture or sputum culture to see what kinds of bacteria are causing any infections your child may have.
- A chest X-ray to take a picture of the chest, including the heart and lungs.
- A CT scan to find any serious disease in the lungs, pancreas, or other organs.
- Blood tests, such as glucose (blood sugar) level and liver function. These tests are to see if there are any complications of cystic fibrosis.
- A stool analysis to see how well your child is absorbing and digesting fat and other nutrients.
- An arterial blood gas analysis to measure the levels of oxygen and carbon dioxide in the blood. This test shows how well the lungs are working.
Cystic Fibrosis - Exams and Tests
Most people who have cystic fibrosis have signs of it when they are children. Tests to diagnose cystic fibrosis can be done at any time—before pregnancy, during pregnancy, right after birth, in childhood, or in adulthood.
The diagnosis of cystic fibrosis requires one of the following:
Article Referenced from WebMD
Diagnosis
A medical history and a physical exam are often the first steps in diagnosing cystic fibrosis, followed by screening or lab tests.The diagnosis of cystic fibrosis requires one of the following:
- Your child has early symptoms. These may include diarrhea that does not go away; large, greasy or very smelly stools; constipation; not wanting to eat; or losing weight. To learn more, see Symptoms.
- A brother or sister who has cystic fibrosis.
- A positive newborn screening test.
- Two positive sweat tests on different dates. Sweat tests measure the level of salt in sweat. People with cystic fibrosis have more than the normal amount of salt in their sweat.
- A positive genetic test for the genetic defect that is known to cause cystic fibrosis. This testing can be done using blood or a sample from the mother's womb before birth (chorionic villus sampling or amniocentesis).
- An abnormal nasal potential difference test. This test uses electrodes on the lining of the nose to see how well salts flow into and out of cells
Article Referenced from WebMD
Sunday, June 15, 2014
How is Sarcoidosis Diagnosed?
There is no single way to diagnose sarcoidosis, since all the symptoms and laboratory results can occur in other diseases. For this reason, your doctor will carefully review your medical history and examine you to determine if you have sarcoidosis. The main tools your doctor will use to diagnose sarcoidosis include:
- Chest X-rays to look for cloudiness (pulmonary infiltrates) or swollen lymph nodes (lymphadenopathy).
- CT scan to provide an even more detailed look at the lungs and lymph nodes than provided by a chest X-ray.
- Pulmonary function (breathing) tests to measure how well the lungs are working.
- Bronchoscopy to inspect the bronchial tubes and to extract a biopsy (a small tissue sample) to look for granulomas and to obtain material to rule out infection. Bronchoscopy involves passing a small tube (bronchoscope) down the trachea (windpipe) and into the bronchial tubes (airways) of the lungs.
What are Granulomas?
A granuloma is a small area of inflammation in tissue. Granulomas are most often the result of an infection and most frequently occur in the lungs, but can occur in other parts of the body as well. They typically cause no signs or symptoms and are found incidentally on a chest X-ray done for some other reason.
The most common cause of lung granulomas in the United States is histoplasmosis, a fungal infection that primarily affects the lungs. People who acquire pulmonary histoplasmosis that results in a lung granuloma have almost always spent some time in the Ohio Valley or the upper Midwest. Most people with pulmonary histoplasmosis never suspect they have the disease because signs and symptoms are rare.
Although granulomas due to histoplasmosis are noncancerous (benign), they may resemble cancer on an X-ray, especially if they haven't calcified — over time, granulomas become calcified and have the same density as bone, making them more clearly visible on an X-ray.
A doctor may make a diagnosis of granuloma by chest X-ray or, if the granuloma is not apparently calcified, by computerized tomography (CT), which can detect the calcium that isn't evident on the chest X-ray. The images of affected tissue usually show scarring and calcification characteristic of a granuloma. Granulomas almost never require treatment or even follow-up chest X-rays.
Article referenced from mayoclinic.org
Article referenced from mayoclinic.org
What is Sarcoidosis?
Sarcoidosis is an inflammatory disease that affects multiple organs in the body, but mostly the lungs and lymph glands. In people with sarcoidosis, abnormal masses or nodules (called granulomas) consisting of inflamed tissues form in certain organs of the body. These granulomas may alter the normal structure and possibly the function of the affected organ(s).
Article Referenced from WebMD
Article Referenced from WebMD
Saturday, June 7, 2014
How Is Pulmonary Fibrosis Treated?
The treatment options for idiopathic pulmonary fibrosis are very limited. There is no evidence that any medications can help this condition, because scarring is permanent once it has developed. Lung transplantation is the only therapeutic option available, but this is usually reserved for advanced cases. At times, this diagnosis can be difficult to make even with tissue biopsy reviewed by pathologists with specific experience in this field. Research trials using different drugs that may reduce fibrous scarring are ongoing. Because some types of lung fibrosis can respond to corticosteroids (such as Prednisone) and/or other medications that suppress the body's immune system, these types of drugs are sometimes prescribed in an attempt to decrease the processes that lead to fibrosis. When these fail, lung transplantation may be considered for some patients.
Article Referenced From WebMD.
How Is Pulmonary Fibrosis Diagnosed?
Pulmonary fibrosis is suggested by a history of progressive shortness of breath with exertion. Sometimes, during examination of the lungs with a stethoscope, the doctor can hear crackling sounds in the chest. The chest X-ray may or may not be abnormal, but a special X-ray test called a high-resolution CAT scan will frequently demonstrate abnormalities. Lung function testing is distinctly abnormal.
Continue reading below...
The diagnosis can be confirmed by lung biopsy. An open surgical biopsy, meaning that the chest wall must be surgically opened under general anesthesia to remove a portion of lung tissue, may be necessary to obtain enough tissue to make an accurate diagnosis. The removed tissue is examined microscopically by a pathologist to confirm the presence of fibrosis.
Article Referenced From WebMD.
.
What Are Pulmonary Fibrosis Symptoms?
What is Pulmonary Fibrosis?
In a condition known as hypersensitivity pneumonitis, fibrosis of the lungs can develop following a heightened immune reaction to inhaled organic dusts or occupational chemicals. This condition most often results from inhaling dust contaminated with bacterial, fungal, or animal products. Examples include silo fillers disease and pigeon breeders lung disease.
In some people, in fact in most cases, chronic pulmonary inflammation and fibrosis develop without an identifiable cause. Most of these people have a condition called idiopathic pulmonary fibrosis (IPF) that does not respond to medical therapy, while some of the other types of fibrosis, such as nonspecific interstitial pneumonitis (NSIP), may respond to immune suppressive therapy.
Other names for various types of pulmonary fibrosis that have been used in the past include chronic interstitial pneumonitis, Hamman-Rich Syndrome, usual interstitial pneumonitis (UIP) and diffuse fibrosing alveolitis.
Article Referenced From WebMD.
Friday, June 6, 2014
The Purple Ribbon Represents The Awareness and Fight Against More Than "SARCOIDOSIS".
Alzheimer's Disease awareness
Thursday, June 5, 2014
Going on the Lung Transplant List
After testing and interviews have been completed and it’s concluded the patient is a good candidate for a lung transplant, he or she will be listed on regional and national organ recipient lists. A person’s place on the list is determined by the Lung Allocation Score, a complicated calculation that tries to predict two things:
- How long a patient is likely to live without a lung transplant
- How long a patient would be expected to live after receiving a lung transplant
People with higher scores are considered first when organ donors’ lungs become available.
Article Referenced from WebMD.com
Preparing for a Lung Transplant
The evaluation process for a lung transplant is usually long and complicated. First, a doctor refers a patient to a regional transplant center. At the transplant center, doctors, psychologists, social workers, and other staff meet with the person to gather information. This may take place on several visits occurring over many weeks or months.
Besides the patient’s lung condition, the team considers the person’s family and social support, financial situation, psychological makeup, and any other medical conditions. Numerous tests are performed during a lung transplant evaluation, which can include:
- Pulmonary function tests
- Cardiac stress test
- Coronary artery catheterization
- Bone mineral density test
- Chest X-ray
- Computed tomography (CT scan) of the chest
- Blood tests for kidney function and liver function, and a complete blood count (CBC)
- Blood type and antibodies present in the blood, for matching against potential organ donors
What is a Lung Transplant?
A lung transplant is an effective treatment for disease that has destroyed most of the lungs’ function. For people with severe lung disease, a transplant can bring back easier breathing and provide years of life. However, lung transplant surgery has major risks and complications are common.
Who May Need a Lung Transplant?
Most people with severe, end-stage lung disease can be considered for a lung transplant. The procedure should be considered when someone seems likely to die without the surgery and no other options are available. A lung transplant can also be considered in people whose lung disease is so severe that they can no longer enjoy life.
The most common lung diseases for which people undergo lung transplant are:
- Chronic obstructive pulmonary disease (emphysema and chronic bronchitis)
- Idiopathic pulmonary fibrosis
- Cystic fibrosis
- Idiopathic pulmonary arterial hypertension
Among people with these conditions, lung transplant reasons can vary. For example, in emphysema, lung tissue is destroyed by smoking; in idiopathic pulmonary fibrosis, scar tissue replaces healthy lung.
Lung transplant centers may hesitate when considering people over age 60 or 65 for lung transplant.
Article Referenced from WebMD.com
Tuesday, June 3, 2014
What Are the Symptoms of Sarcoidosis?
What Are the Symptoms of Sarcoidosis?
The symptoms of sarcoidosis can vary greatly, depending on which organs are involved. Most patients initially complain of a persistent dry cough, fatigue, and shortness of breath. Other symptoms may include:
- Tender reddish bumps or patches on the skin.
- Red and teary eyes or blurred vision.
- Swollen and painful joints.
- Enlarged and tender lymph glands in the neck, armpits, and groin.
- Enlarged lymph glands in the chest and around the lungs.
- Nasal stiffness and hoarse voice.
- Pain in the hands, feet, or other bony areas due to the formation of cysts (an abnormal sac-like growth) in bones.
- Kidney stone formation.
- Enlarged liver.
- Development of abnormal or missed heart beats (arrhythmias), inflammation of the covering of the heart (pericarditis), or heart failure.
- Nervous system effects, including hearing loss, meningitis, seizures, or psychiatric disorders (for example, dementia, depression, psychosis).
In some people, symptoms may begin suddenly and/or severely and subside in a short period of time. Others may have no outward symptoms at all even though organs are affected. Still others may have symptoms that appear slowly and subtly, but which last or recur over a long time span.
Info Taken From Med Web Site
Monday, June 2, 2014
What is a Auto Immune Disease?
Our bodies have an immune system, which is a complex network of special cells and organs that defends the body from germs and other foreign invaders. At the core of the immune system is the ability to tell the difference between self and nonself: what's you and what's foreign. A flaw can make the body unable to tell the difference between self and nonself. When this happens, the body makes autoantibodies (AW-toh-AN-teye-bah-deez) that attack normal cells by mistake. At the same time special cells called regulatory T cells fail to do their job of keeping the immune system in line. The result is a misguided attack on your own body. This causes the damage we know as autoimmune disease. The body parts that are affected depend on the type of autoimmune disease. There are more than 80 known types.
Sunday, June 1, 2014
What is sarcoidosis?
What is sarcoidosis?
Sarcoidosis is a disease that results from a specific type of inflammation of tissues of the body. It can appear in almost any body organ, but it starts most often in the lungs or lymph nodes.
The cause of sarcoidosis is unknown. The disease can appear suddenly and disappear. Or it can develop gradually and go on to produce symptoms that come and go, sometimes for a lifetime.
As sarcoidosis progresses, microscopic lumps of a specific form of inflammation, called granulomas, appear in the affected tissues. In the majority of cases, these granulomas clear up, either with or without treatment. In the few cases where the granulomas do not heal and disappear, the tissues tend to remain inflamed and become scarred (fibrotic).
Sarcoidosis was first identified over 100 years ago by two dermatologists working independently, Dr. Jonathan Hutchinson in England and Dr. Caesar Boeck in Norway. Sarcoidosis was originally called Hutchinson's disease or Boeck's disease. Dr. Boeck went on to fashion today's name for the disease from the Greek words "sark" and "oid," meaning flesh-like. The term describes the skin eruptions that are frequently caused by the illness.
Article taken from medicine.net
Subscribe to:
Comments (Atom)